When I lifted my arm to tousle my already frizzed hair, the neurologist—the fourth doctor I’d seen in the hopes of finding some panacea that would abolish my migraines—eyed the matchstick-shaped protrusion in my bicep almost accusingly, not so much accusing the matchstick per se as condemning me for allowing it to take up residence in my body. The last doctor I saw, before I was on birth control, assumed that my migraines must be hormonal, regardless of there being no correlation between the onset of a migraine and the timing of my cycle. This new doctor grilled me about my birth control, asking leading question after leading question in hopes of arriving at the answer that the birth control implant is the reason that I think I know what it would be like to be struck by a flash grenade. As if my migraines hadn’t started before menarche. As if they hadn’t stalked me through the early, unmedicated days of womanhood and been undeterred when I began taking The Pill. I had almost eight years of migraines before I decided to get the birth control implant.
I describe my pain to friends and doctors in the same way, and that way is: defensively. I hedge and apologize and shoo away sympathy, afraid of taking too much and deserving too little.
People are tired of hearing about pain, especially women’s pain, and I hate to tire people. I also feel a certain guilt at the fact that no doctor has been able to fix me. To many, this fact suggests that I am either exaggerating or entirely manufacturing my pain. That, in more ways than one, my migraine pain is all in my head. One doctor, a woman this time, and a former practitioner at a neurology clinic, told me that she, too, had occasional headaches and that women just have to learn to live with them. I was in her office after spending the better part of three days in my darkened dorm room, leaving only to vomit and then dry retch in the bathroom I shared with thirty other girls that year.
My experience is not unique and pales in comparison to what some women have gone through in working to say or solve their pain. There is a sense that women deserve their pain—Eve’s curse upon all of us—but even the idea that pain is an earned punishment does not bestow legitimacy.
Hysteria. This word haunts women from within and without whenever there is doubt about the cause of a physical symptom. The idea originated with Hippocrates’s idea of the “wandering womb.” He believed that the uterus could become dislodged from its appropriate setting and tour the rest of the female body, wreaking havoc wherever it went. When he sees me in pain, my partner jokingly asks where my uterus is at the moment.
The autopsy would eventually put an end to the wandering womb theory, but hysteria remained alive and well, morphing into a psychological explanation for any distress experienced by a woman. Though we now know that women diagnosed with hysteria were likely suffering from a range of severe illnesses, it was taken exceptionally lightly by male physicians. André Brouillet’s 1887 painting “A Clinical Lesson at the Salpêtrière” depicts the famous neurologist Jean-Martin Charcot lecturing with a swooning female patient, Marie “Blanche” Wittman, draped over one forearm.
The uterus—and, by extension, fertility—have long been at the heart of understandings of female pain, both in Abrahamic religions’ description of pain in childbirth as a punishment for original sin and in physicians’ use of the word “hysteria”—derived from the Greek word for uterus—to describe a wide range of physical and psychological discomfort in women. Hysteria was for many years a legitimate diagnosis. These days, you’d be hard pressed to find a woman who hasn’t had the term hurled at them during an argument.
Gabrielle Jackson, author of Pain and Prejudice, has found the legacy of such thinking in the treatment of endometriosis—a disorder in which uterine lining develops outside the uterus, causing extreme pain. This pain is other than my own, and I cannot imagine it. But I can imagine the scorn and doubt that women with endometriosis—or endo, which it is not-so-lovingly called by those unfortunate enough to be so familiar—experience when they express their pain. Having your pain diminished or disbelieved means you don’t get much of a say in how it is treated.
“Women often privilege symptomatic relief, and want to be able to go about their everyday lives,” Jackson writes. “Clinicians instead privilege fertility.”
As so often happens, the potential for new life supersedes the life that is already here.
Jackson continues, “One of the reasons for that is probably to do with their training, and might go back to the fact that we haven’t incorporated women’s perspectives and knowledge about their bodies into science and medicine.”
It isn’t an imagined issue: In the U.S., men wait an average of forty-five minutes before receiving pain-relieving drugs for acute abdominal pain, while women wait an average of sixty-five minutes. But why, in an American culture that largely denies the presence of gender inequality, have we failed to hear women’s voices when it comes to the treatment of their bodies?
There are many reasons for this, with one of them being that women still make up just over one-third of practicing physicians. Beyond that, the high-prestige specialties are even more difficult for women to enter, with only less than ten percent of neurosurgeons being women.
Something else, though, might better explain why women’s pain is such a nonissue to clinicians: Women and pain are a winning cultural combo. It just makes sense for women to suffer and to complain about suffering.
I do not intend to claim that men do not feel pain and its social repercussions, including an inability to express their pain and maintain certain masculine identities. However, the feminization of pain—and the “paining” of women—means that women’s experiences of these things are just different.
Let this sink in: women in pain are significantly more likely than men in pain to receive sedatives rather than analgesics. The act of complaint, rather than the subject of it, receives treatment. This is largely because clinicians believe men to be more stoic. A large body of literature demonstrates that clinicians expect that women greatly exaggerate their pain, so they treat the ability to exaggerate by medically subduing women.
In other words, my eleven is understood as a man’s four. This problem is even worse for Black women, whose pain is even more disbelieved. Black pain patients receive less pain medication than their white counterparts. One reason for this is that, to this day, many medical students and clinicians believe that Black people have thicker skin than white people and therefore feel less pain. In 2012, forty percent of first- and second-year medical students believed this. Another reason is that many clinicians think Black patients will abuse pain medications.
But as long as my pain keeps me acting like a sensitive woman and can be blamed on my female physiology, and as long as a Black woman’s pain can be understood within a framework of dominant racist stereotypes, there is little sociocultural incentive for these pains to be heard, understood, treated. For those of us with chronic pain, this means we spend our whole lives trying to make ourselves clear.
Elaine Scarry writes, “It is the intense pain that destroys a person’s self and world, a destruction experienced spatially as either the contraction of the universe down to the immediate vicinity of the body or as the body swelling to fill the entire universe.”
She also writes, “Physical pain always mimes death and the infliction of physical pain is always a mock execution.”
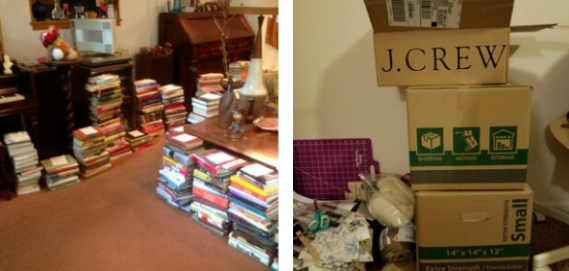
But what happens when people define you by your pain and their disbelief in it? Or when your pain begins to eat away acid-like at the rest of your life? Scarry’s characterization of pain would seem to mean that people with chronic pain live death like zombies. The thing is, though, you don’t feel death, but you do feel pain. This sounds obvious, but chronic pain is chronic feeling.
Perhaps this is why chronic pain diagnoses like fibromyalgia are feminized in popular discourse. People see feeling and think woman. For people who aren’t women, this is a violent misidentification. For women, this just makes sense. Just as hurting makes a person womanly in some eyes, being a woman is embodying pain: childbirth, period cramps, headaches, heartbreak.
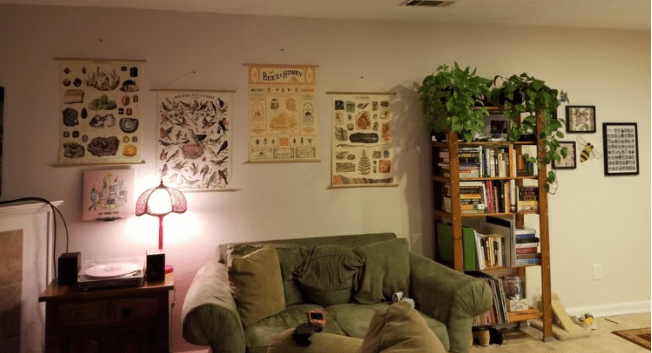
The problem here is the reduction that comes with such constructed one-to-one ratios between femaleness and painfulness. This ratio implies that woman and pain are one and the same. But pain does not constitute a person even as it may reduce the circumstances of personhood. A migraine may keep me in bed, but it doesn’t erase me. I may fade out temporarily from the worlds of others, but I still exist to myself. I am hurting, not dead. There is still a me to feel pain.
This is what makes the world’s exhaustion with female pain so frustrating. I can talk all day long about everything under the sun, but as soon as I mention my pain, no one cares to listen. Suddenly, all of me is collapsed into one part of my experience, of my identity, and I no longer deserve a voice.
It would be foolish of me to believe this voicelessness is unique to or more severe in my case than it is for millions of other women. Women of color, queer women, trans women, and people with uteruses who may not identify as women have historically not been empowered to make themselves heard. I understand the privilege that allows me to write this essay and have it be read. But pain is common to all of us, and I hope that my voicing an unpleasant issue will help to make space for other women to share their own pain. Such expression, from all of us, will be the thing that proves we are more than our pain.